Repetitive Stress Recovery: A Step-by-Step Guide to Healing Soft Tissue Injuries
Repetitive stress injuries (RSIs) can sneak up slowly but have a major impact on your day-to-day life- especially if your work or hobbies require repeated motions. Whether you're a musician, climber, ceramicist, office worker, or therapist yourself, you may have experienced the frustration of nagging pain that doesn’t go away with rest alone.
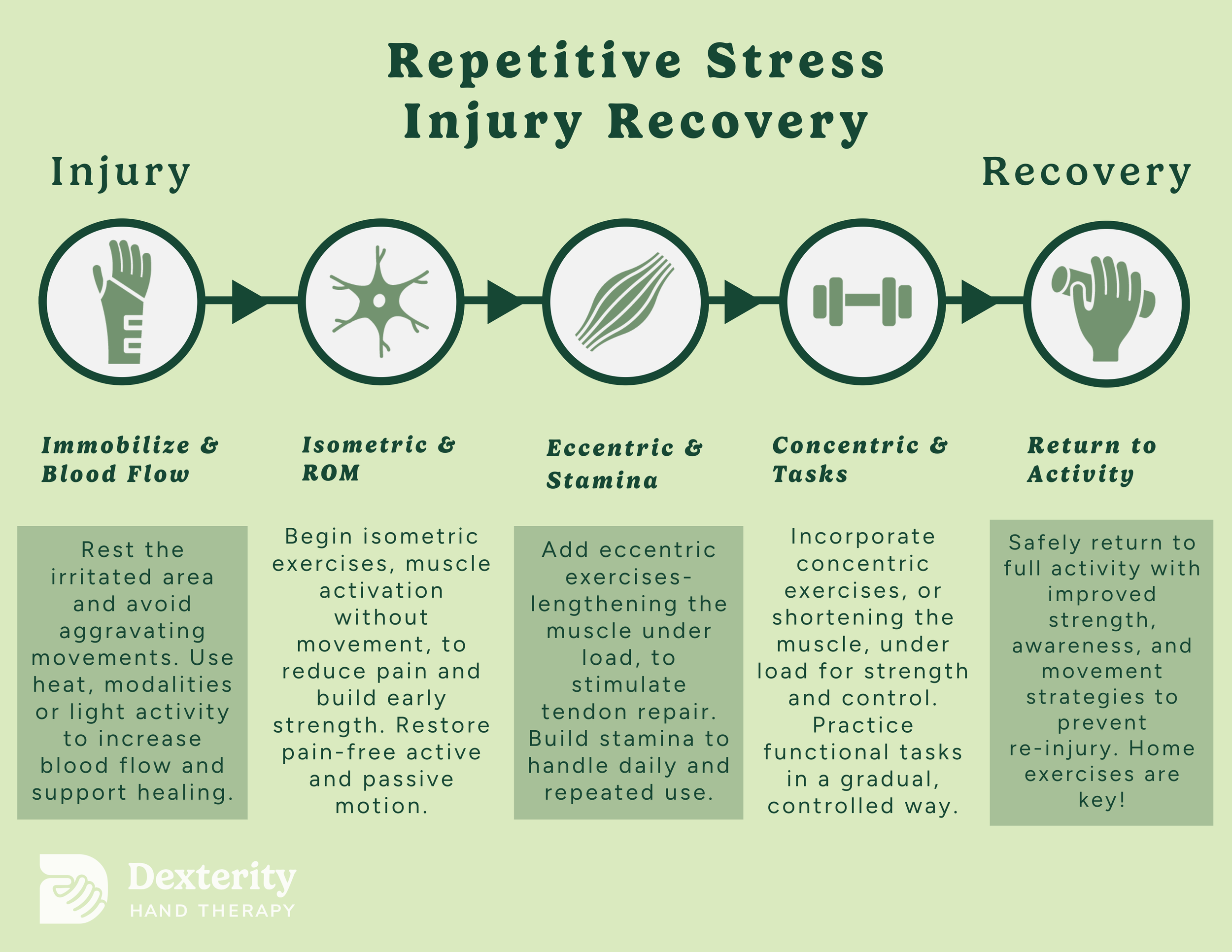
Fortunately, there's a structured, research-backed path to recovery. In this post, we’ll explore the five essential phases of RSI rehabilitation, with strategies rooted in current peer-reviewed research. Understanding the purpose of each stage, and what your body needs at that point, can help you recover more fully and avoid reinjury.
Stage 1: Immobilize & Increase Blood Flow
When an RSI first flares up, the primary goal is to calm things down. This is not the time to push through the pain! in fact, continuing to load irritated tissue can worsen the damage.
Short-term immobilization or modified activity helps prevent further strain on inflamed tissues. Sometimes, in more difficult cases, this can mean wearing a custom orthosis to prevent irritating movement for a couple of weeks. However, this also means strategic avoidance of aggravating movements while continuing general movement elsewhere.
At the same time, increasing blood flow to the affected area helps speed healing by delivering oxygen and nutrients. Gentle heat, soft tissue massage, or active recovery techniques (such as light aerobic movement) can all be effective. In addition, modalities such as ultrasound and laser therapy can help increase blood flow. A 2021 study by Millar et al. emphasized the role of inflammatory processes in tendon healing, reinforcing that early interventions supporting circulation and tissue metabolism are crucial for repair.
This is also the stage where patient education is most important. Learning what movements to avoid, and how to modify posture or technique, can protect the tissue while it heals and lay the groundwork for long-term recovery. It’s most important to educate yourself on the triggers causing the irritation in the first place.
Stage 2: Isometric Loading & Restoring Range of Motion
As pain and inflammation begin to settle, the next goal is to gently reintroduce load to the tissue, starting with isometric exercises.
Isometric contractions involve muscle activation without a change in muscle length. Imagine pushing your hand against a wall and holding that contraction without actually moving the joint- this is an isometric exercise. Research by Rio et al. (2015) found that isometric loading can reduce pain and improve tendon function early in rehabilitation, especially for tendinopathies.
These static contractions allow the muscle and tendon to begin bearing load again in a controlled, non-aggravating way. They’re especially helpful in reducing pain-related inhibition, a phenomenon where pain causes muscles to “shut down” or underperform.
At the same time, you’ll want to gently restore joint mobility by working on both active (self-initiated) and passive (outwardly initiated) range of motion. Maintaining or regaining full motion is essential to prevent stiffness, improve circulation, and prepare for future loading. Malliaras et al. (2015) highlight that improving pain-free range of motion alongside early loading is critical in optimizing long-term outcomes in tendon and overuse injuries.
Stage 3: Eccentric Strengthening & Building Stamina
Once you can comfortably tolerate isometric contractions and have restored range of motion, the focus shifts to eccentric strengthening.
Eccentric exercises involve controlled lengthening of the muscle under load. For example, slowly lowering a dumbbell during a bicep curl. This type of loading is particularly effective in remodeling tendon structure, stimulating collagen synthesis, and improving tendon stiffness and strength.
In fact, eccentric loading has become a gold standard in chronic tendon rehab, especially for conditions like lateral epicondylitis (tennis elbow) or Achilles tendinopathy.
A 2015 randomized controlled trial by Beyer et al. showed that both heavy slow resistance and eccentric-only exercises significantly improved outcomes for patients with Achilles tendinopathy.
This stage also introduces gradual endurance training. Repetitive stress injuries aren’t just caused by weakness, they’re often the result of insufficient stamina for the demands of a task. Building up time-under-tension and resistance to fatigue helps ensure the muscle-tendon unit can handle your daily activities or performance goals without flaring up again.
Stage 4: Concentric Loading & Task-Specific Training
Once eccentric strength and endurance are in place, it's time to incorporate concentric exercises. These are movements where the muscle shortens under tension. These help build power and control, improving your ability to generate force efficiently.
While concentric exercises are common in traditional strength training (e.g., lifting a weight during a bicep curl), they’re particularly important during task-specific rehab. This is the bridge between rehab and real-life performance.
For example, a guitarist might work on controlled plucking or strumming patterns with proper posture and muscle engagement. A climber might practice controlled gripping and pulling in progressive sequences. This phase builds confidence and prepares the nervous system for complex, coordinated actions.
As Scott et al. (2020) emphasized, combining strengthening with task-specific retraining is key in helping athletes and performers return to sport or craft without symptoms.
At this stage, sessions often become more personalized. Functional drills, real-world simulations, and graded exposure help refine movement strategies and prevent maladaptive patterns from resurfacing.
Stage 5: Return to Full Activity & Long-Term Maintenance
The final stage of recovery is when you’re back to doing what you love- without pain, hesitation, or fear of reinjury. But this isn’t the time to abandon your movement habits or strength routine.
In this phase, patients resume full activity with improved awareness, refined mechanics, and enhanced strength and endurance. Importantly, you’ll continue to manage load over time while being mindful of volume, intensity, and recovery.
Docking & Rio (2019) describe tendon health as a continuum, noting that even after symptoms resolve, structural changes may persist. Ongoing load management and movement education are essential to keep symptoms from returning.
Self-monitoring plays a big role here. Being able to identify early signs of overload: such as fatigue, tightness, or low-level pain. You will also need to modify activity accordingly is the foundation for long-term success.
Some patients benefit from occasional “tune-ups” or check-ins with a therapist to reassess form, adjust training plans, or manage flare-ups before they escalate.
A Quick Summary of the 5 Phases
Final Thoughts
Repetitive stress injuries don’t resolve with rest alone. Recovery requires a thoughtful, step-by-step approach that supports the body’s natural healing processes while retraining strength, movement, and endurance.
Whether you’re a creative professional, athlete, or simply trying to get back to pain-free work and life, working with a skilled rehabilitation specialist can make all the difference. Recovery is not just about healing, it's about coming back smarter, stronger, and more resilient than before.
References
Beyer, R. et al. (2015). Heavy slow resistance versus eccentric training as treatment for Achilles tendinopathy. Am J Sports Med, 43(7), 1704–1711. https://doi.org/10.1177/0363546515584760
Docking, S. I., & Rio, E. (2019). Tendon structure and health: What clinicians should know. Br J Sports Med, 53(3), 163–165. https://doi.org/10.1136/bjsports-2018-099845
Malliaras, P. et al. (2015). Achilles and patellar tendinopathy loading programmes. Sports Med, 45(11), 1469–1487. https://doi.org/10.1007/s40279-015-0364-2
Millar, N. L. et al. (2021). Inflammation and tendinopathy: No longer a paradox. Br J Sports Med, 55(4), 203–205. https://doi.org/10.1136/bjsports-2020-103408
Rio, E. et al. (2015). Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. Br J Sports Med, 49(19), 1277–1283. https://doi.org/10.1136/bjsports-2014-094386
Scott, A. et al. (2020). Sports and exercise-related tendinopathies: A review of selected topical issues. Br J Sports Med, 54(5), 302–308. https://doi.org/10.1136/bjsports-2018-099028